Many health care systems across Georgia have no plans to mandate coronavirus vaccines for frontline workers, despite increasing infections caused by a variant that reportedly spreads as easily as chickenpox.
Nearly 60 major medical organizations called this week for mandatory vaccines for most health care workers, and an internal report surfaced from the U.S. Centers for Disease Control and Prevention that described the highly contagious nature of the Delta variant that is causing the latest increase. Even so, most health care systems in Georgia say that while they will require masks and follow other safety protocols, they’ll continue letting employees decide on their own about vaccinations.
Vaccination rates among health care workers vary widely across the state, although a majority of employees of many major providers have received at least one shot, The Atlanta Journal-Constitution found.
At Children’s Healthcare of Atlanta, where many patients are too young to get the vaccine themselves, one-quarter of clinical and non-clinical employees have not been inoculated. At Albany-based Phoebe Putney Health System, the epicenter of one of the first COVID-19 outbreaks in Georgia, 45% of employees have not been fully vaccinated. At Emory Healthcare in Atlanta, less than one-third of the workforce is unvaccinated.
Nationwide, one in four hospital workers who have direct contact with patients had not yet received a single dose of a COVID-19 vaccine by the end of May, according to an analysis by Medscape Medical News and WebMD of data that 2,500 hospitals reported to the federal government. The data showed an even greater proportion of unvaccinated workers — one in three —at the nation’s 50 largest health care providers.
Georgia public health officials and the CDC said they do not track vaccination rates for frontline workers at hospitals and nursing homes.
Vaccine resistance among health care workers is no surprise, said Dr. Harry Greenspun, chief medical officer for Guidehouse, a management and consulting firm based in Virginia.
“People forget that health care workers are people,” Greenspun said. “We tend to appropriately laud our frontline workers, and there’s a lot of heroic work going on. But fundamentally health care workers are just people, and we shouldn’t be surprised that still a large number have to be reminded to be vaccinated and they have the attitudes reflected by the communities they come from.”
‘Protect those under our care’
The debate over mandates comes amid an abrupt rise in new coronavirus infections. Georgia’s seven-day rolling average of probable and confirmed coronavirus cases is at its highest point since Feb. 20, when the state’s most recent surge was waning, and a growing number of hot spots have emerged in rural counties where vaccination rates are staggeringly low.
Statewide, only 40% of the population is fully vaccinated, compared to 50% across the nation.
But as the latest uptick arrived, some health care providers in Georgia took action.
Deke Cateau, chief executive of A.G. Rhodes, an Atlanta nonprofit that operates three nursing homes, issued a mandate this week: employees must be vaccinated by Oct. 1. Cateau had hoped to avoid such a dictate, but was uncomfortable with just 60% of the staff taking the vaccine voluntarily.
“It became an ethical and moral imperative that we take action because we cannot go back to what happened last year,” Cateau said, referring to the widespread deaths in nursing homes and other long-term care facilities. “We’re all tired. We’re all at our brink, and we simply can’t go back to that. . . . We have to protect those under our care.”
PruittHealth, one of Georgia’s largest nursing home chains, announced Tuesday that, effective Oct. 1, all administrators and directors of health services, along with other managers and corporate employees must be vaccinated. CEO Neil Pruitt said the company would meet with other employees before deciding on a company-wide mandate.
“Low vaccination rates are fueling the current wave of COVID-19 our country is experiencing, and we must trust in the science that was developed to protect us,” Pruitt said.
Atria Senior Living decided in January to require its 10,000 employees at assisted living centers across the country to get vaccinated, said John Moore, chairman and CEO. Among the company’s 215 employees in metro Atlanta, Moore said, 98.6% are vaccinated.
Piedmont Healthcare, one of Georgia’s largest health care systems, is requiring its doctors and other providers, including nurses and physician assistants, along with executives and new employees, to be vaccinated by Sept. 1. Other employees will have to be vaccinated in the “near future,” Piedmont said this week.
“It became an ethical and moral imperative that we take action because we cannot go back to what happened last year."
Richard Gerakitis, a labor and employment law attorney in Atlanta, said it was only a matter of time before more health care providers adopted the mandate.
Most want to wait until the U.S. Food and Drug Administration gives full authorization to the vaccines, he said. So far, the FDA has given only emergency-use authorizations to the vaccines manufactured by Pfizer, Moderna and Johnson & Johnson.
“Employers could mandate it now but I think they prefer to have full use authorization,” Gerakitis said.
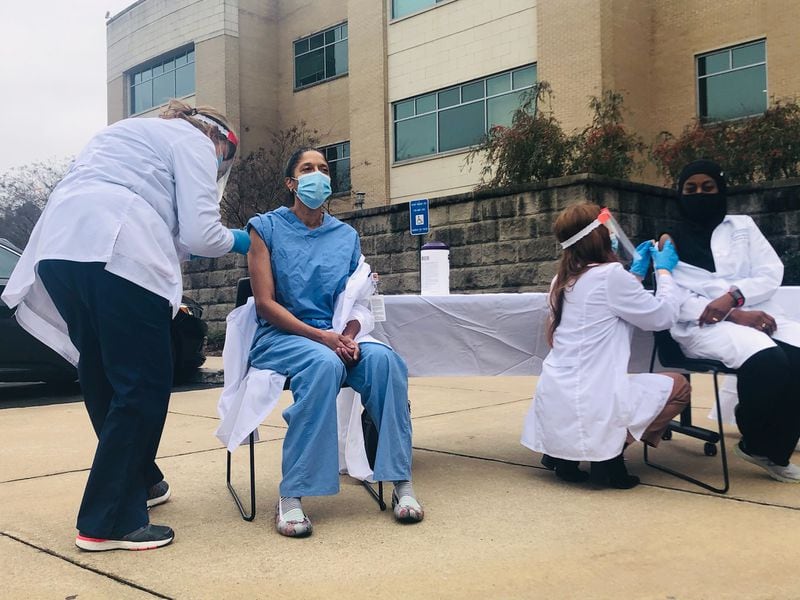
Credit: Christine Tannous / Christine.Tannous@ajc.com
Credit: Christine Tannous / Christine.Tannous@ajc.com
Mixed response
Some hospitals feared an abrupt mandate could trigger a backlash among employees at a time when angst about the shots is at an all-time high. That applies especially outside the state’s urban regions, said Jimmy Lewis, CEO of HomeTown Health, an advocacy group for rural hospital providers.
Other providers told the Journal-Constitution that they are still weighing their options.
Wellstar Health System said in a statement that it is “actively evaluating the latest guidance from public health authorities and clinical experts.” But for now, it is not requiring employees to be vaccinated.
At Emory Health, officials said the hospital had strongly encouraged but not yet required the vaccination for employees, “as we previously communicated that we planned to require vaccination upon full FDA approval.”
Because of the spike in cases, however, “we are currently reviewing this plan and will communicate any potential change to our team members first.”
Meanwhile, health care providers may need to get creative to persuade vaccine holdouts within the profession, said Greenspun, the chief medical officer for Guidehouse.
Publicity campaigns and raffles won’t work for them, he said.
“These health care workers are not going to be influenced by the American Hospital Association,” he said. “They are much more interested in their church and community leaders and what other folks like that have to say. Obviously, that’s the kind of outreach that has to be done.
“Also, employers need to be tapping into that self-interest in people and telling them, ‘Look, you are putting your parents at risk, you are putting your kids at risk.’”
/cloudfront-us-east-1.images.arcpublishing.com/ajc/NSZWU36A2ZENFO44MVAPXOAZRQ.jpg)